AUSTIN — Amy Pratt drove her severely disabled son, Quinten, four-plus hours to Children’s Medical Center Dallas only to learn the insurance company that Texas hired to care for him had suddenly denied payment for an important procedure, one that could potentially save the 9-year-old’s life.
In El Paso, 11-year-old Rudy Smith lost most of the therapy services that helped him cope with cerebral palsy and a severe form of epilepsy, which plagues him with 50 to 100 seizures a day. His mother says she’s having trouble getting prescriptions filled, and the insurance company keeps sending her incorrect or faulty medical supplies.
Arlington resident Blakley Hernandez is considering moving to another state because her son, Reid, a 3-year-old with a form of dwarfism, can no longer see specialists who were planning surgeries to fix his legs, which are bowing outward.
These children are among 6,000 of Texas’ most vulnerable patients whose lives may have been put at risk by the state’s effort to cut Medicaid costs, their parents say. Lawmakers handed off their children’s care to private companies and nonprofit hospitals in November.
Recent changes to the Medically Dependent Children Program — which provides aid for children whose maladies are so extreme that they require round the clock “nursing facility level care” — have caused alarming and widespread problems, a Dallas Morning News investigation found.
The problems go far beyond agonizing red tape and hours of haggling with doctors and insurers over the phone. Parents say that life-or-death prescriptions aren’t being filled in a safe time frame and that children are losing access to specialists and nurses who are trained to treat rare and chronic disorders. Procedures and exams are being denied, they say, and impassioned complaints to the state are going nowhere.
“There are tons of cuts that could be made, but [Texas lawmakers] chose to target children and families that don’t have a voice,” said Pratt, who got her son in for that procedure, but only after spending hours on the phone with Superior Health Plan and firing off dozens of frantic emails to lawmakers.
Quinten, who has autism and a complex genetic disorder that stunts him mentally and wreaks havoc on his heart, lungs and bowels, needed to fast before his procedure. Because of the delay, he went 18 hours without food or water before finally being admitted for the surgery, his mother said.
“You try to explain to a 9-year-old autistic boy — sorry, you can’t eat because someone has decided this isn’t worth it,” said Pratt, the mother of five who drove to Dallas from Canyon Lake, a town tucked between Austin and San Antonio.
For years, the Medically Dependent Children Program has saved and improved the lives of countless children like Quinten, who would otherwise be permanently stuck in a hospital bed or dead. But in November, state health officials overhauled the system, rolling out a new program dubbed STAR Kids, which encompasses both severely disabled children and nearly 160,000 other disabled children.
Championed in 2013 by Republican Sen. Jane Nelson of Flower Mound, the changes allowed the state to cut costs and streamline health care by handing off administration of Medicaid services for medically vulnerable children to private health groups called managed care organizations, or MCOs.
Instead of the state wrangling bills from thousands of doctors, it cuts a few big checks to the MCOs, which decide how much they will pay doctors and which services they will cover. One way for MCOs to turn a profit is to eliminate services they view as unnecessary. But parents say they’re cutting services they desperately need.
The STAR Kids rollout has been a mess, according to state records and interviews with more than a dozen families and several health care providers.
Complaints flooding in
The Health and Human Services Commission, which administers Medicaid programs, has received more than 730 complaints about STAR Kids since it began three months ago, according to an agency spokeswoman.
The commission is working to dig through those complaints, which flooded in from patients, their families and health care providers.
“We want families to contact us and raise flags if they’re having issues,” spokeswoman Carrie Williams said. “We have a team standing by to help families because we know these services are critical, and we want to resolve issues as quickly as possible.”
The commission denied an open-records request by The News to review hundreds of those complaints, citing patient privacy.
But a group of concerned parents, who formed the nonprofit Protect TX Fragile Kids, say they’ve tried to get help from the state and their legislators. The group has about 1,500 members and has launched email and Twitter campaigns, but it says they’re not being heard.
“What we found was there were far more questions there than they had answers to,” said Hannah Mehta of Flower Mound, director of the nonprofit. “We quickly realized, and HHSC told us, that if there’s no political will, nothing is going to change.”
Mehta’s son Aiden is a triplet with a combination of birth defects including digestive and respiratory issues. She says children like Aiden are too fragile to be adequately treated in a managed care model.
Mehta reached out to her senator, Nelson, author of the 2013 measure that her group says has imperiled thousands of children. Nelson listened, she said, but they have seen no improvements.
Nelson has asked health officials for detailed updates and is working with them to suss out solutions to problems with the STAR Kids rollout, according to her spokeswoman.
“I have met with families, listened to hours of testimony and am carefully monitoring this transition to ensure that children receive the services they need,” Nelson said in a prepared statement. “I am working with the agency to assist every individual who has contacted my office.”
Before the Health and Human Services Commission launched the change, it said parents would be grandfathered into the program for the first six months, so-called “continuity of care,” which meant, among other things, they could keep their doctors.
But that promise has been broken, Mehta said, because the insurance companies are denying services and prescriptions. Many doctors won’t work with the companies the state picked because they don’t pay for procedures in a timely manner or correctly.
“We have had a number of families who have had critical medication denied,” she said. “We’ve had families who have had some surgical delays and have been told, sorry, you’re not in network.”
Kids in danger
Southlake mother Natalie Gregory had to switch from her preferred doctors in Tarrant County who knew Christina, her 2-year-old with a disorder in which her brain forgets to tell her lungs to breathe. They are forced to travel farther to a smaller network of providers in Dallas County.
Rudy Smith’s mother, Erica Smith, says she’s a nervous wreck because their new insurer, Amerigroup, has denied his epilepsy medications and keeps sending the wrong medical supplies and formula, which is how her son eats.
“If you miss a dose of epilepsy medication, you could die,” she said.
Amerigroup did not respond to a request for comment.
Like many others, Smith has had trouble obtaining approved medications because they aren’t readily available at pharmacies such as Walgreens; instead, they must be mixed by a certified compounding pharmacist. And she says Amerigroup, their assigned MCO, won’t authorize a prescription until the medicine is 90 percent gone — sometimes just a few days before he’s out.
“We’ve had it happen before, in the past, where you go to fill his prescription and they have to order it,” Smith said. “Well, what if they can’t get it in time? You have to go to the emergency room.”
Heidi Waters of Austin said her 14-year-old son, Tucker, was “categorically denied” for spinal surgery that had been approved but happened to be scheduled 15 days after the state transitioned the family to the Superior Health Plan MCO.
That’s not supposed to happen.
“Health plans have to ensure continuity of care and are required to honor existing authorizations,” said Williams, the Health and Human Services spokeswoman.
Attempts to reach a representative of Superior Health Plan, by phone and through the company’s website, were unsuccessful.
Waters said it came as a surprise that the company wouldn’t pay for the procedure — which would have installed a pump to push medicine into Tucker’s spinal column, common for growing adolescents who suffer from cerebral palsy.
“They would not even talk with us,” she said. “They wouldn’t take my calls, nothing.”
Their MCO also denied his prescription for Sinemet, a common Parkinson’s medication that’s used to treat people with his condition, said his mother, who is paying out of pocket for the medication.
Tucker was fortunate that his father’s job provided decent primary insurance, which is common. The Medicaid waiver helps poor families but is also designed to pick up the costs that go well beyond what private insurers cover. The idea is that families whose children require 24/7 care shouldn’t have to go bankrupt to keep their kids alive and out of a nursing facility.
Waters didn’t want to wait on the spinal surgery, so rather than fight with Superior Health Plan and the state, she paid the remaining balance.
“We had the money to pay the overage,” she said. “It’s our kid. We’re going to pay it, but what about all these poor parents who have kids, sick like Tucker, but they don’t have resources?”
A history of problems
STAR Kids is the most recent rollout of a much larger shift in the state’s handling of Medicaid, which is increasingly privatized and dependent on managed care organizations, the big networks to which the state pays a flat rate to handle thousands of patients and doctors.
It was projected to save the state hundreds of millions of dollars, and supporters argued that the MCO model would provide better services for patients.
But documents show the state has known for years that its switch to the MCO model has been fraught with problems.
The state has noted several failures and issues with MCOs, including some hired as part of STAR Kids. Those problems include substandard care, high-needs patients losing access to health care, and health insurers cutting corners or inflating diagnoses to maximize profits.
The most recent findings are tucked in a 510-page Legislative Budget Board report, which Lt. Gov. Dan Patrick, who holds sway over the board, tried to conceal from the public last month.
In 2013, then-Sen. Patrick was a co-author of Senate Bill 7, which prompted the overhaul of a sprawling and complicated network of Medicaid services.
With STAR Health — a different iteration of the managed-care model used for foster children — state analysts found that “high needs children have difficulty getting connected to services they need.”
Even before Nelson’s bill was passed, the inspector general over the state health commission found that a subsidiary of United Healthcare, Evercare, was gaming the system to make more money. The subsidiary was “inappropriately” labeling patients as needing home-based services when they didn’t, the inspector general found.
The News contacted the Texas media relations office of United Healthcare, but it did not comment.
Dissatisfaction with the STAR programs more than doubled among patients in some programs. Patients and families, interviewed by the inspector general’s office in 2012, considered not seeking health care altogether because the services were so poor.
“Members expressed they would prefer to forego their health care to avoid future negative experiences,” the report states.
That’s simply not an option for children who need 24/7 nursing care and could die if something goes wrong with a breathing tube, for instance.
Yet all of these documented failures are happening with STAR Kids, said Kristen Robinson, a nurse with Angels of Care, a pediatric home nursing operation in Sherman.
“We’ve seen at least one kid that I’m aware of that ended up back in the hospital because she couldn’t get the medication she needed,” Robinson said.
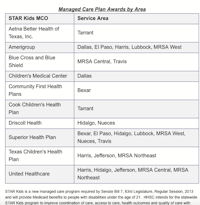
As of Nov. 10, different health insurers manage distinct regions across the state. Under STAR Kids, each has the flexibility to set the rates they’ll pay doctors, many of which won’t work with certain insurers.
Many nursing providers and doctors are reluctant to work with the new system because they’ve been stiffed by the companies before, providers and advocates said.
“Providers are having issues getting paid,” Robinson said. “We’re going through them issue by issue.”
Will it get worse?
Texas health officials confirmed that they’ve fielded reports from doctors who haven’t been reimbursed by the MCOs.
Many of those were related to providers submitting claims with issues — such as one procedure being billed under an arcane service code but the MCO needing it to be billed under a different code — the expected headaches of modern insurance.
But Rachel Hammon, executive director of the Texas Association for Home Care and Hospice, said the blame lies with the state and with the insurers it hired to run STAR Kids.
“They were wholly unprepared to do this, and the kids are suffering the consequences of that,” she said. “You’re playing with their lives. It is super serious.”
And if nothing is changed, children will suffer more, Hammond and others said, because the state’s “continuity of care” period ends soon and insurers will reassess the children to determine what services they can keep and which they deem superfluous.
“MCOs are about cost savings. And they do that by taking services away. It’s going to happen,” said Rebecca Galinsky, a Dallas mother whose son suffers from a connective tissue disorder.
From Scottish Rite Children’s Hospital in Dallas, Galinsky explained how what might sound like tedious paperwork to normal patients became a calamity for her family.
“I never yell at anyone, but I’m yelling at this woman and crying on the phone, having a breakdown because they’re putting his life at risk,” she said about the day in mid-January when doctors denied her son’s back surgery.
Before that surgery, 8-year-old Samuel needed an MRI. But before he could get one, doctors had to remove his cochlear implants. In all, he needed four procedures in a short time.
Galinsky says the family’s private insurance, United Healthcare, covered three of the procedures but not the fourth. But luckily — she thought at first — Cook Children’s Health Plan, Samuel’s Medicaid MCO, agreed to pay for all four.
Then, suddenly, doctors at Cook Children’s Hospital said they couldn’t do any of the procedures. They were worried the hospital would end up eating the cost. Even though Cook Children’s said it would cover the entire operation, the MCO might come back and say no because United Healthcare had said it wouldn’t.
“They told me they won’t provide my son’s surgery because they don’t trust Cook Children’s Hospital MCO to pay,” Galinsky said. “They don’t trust these MCOs because they’ve already been burned.”
Cook Children’s Health Plan couldn’t provide comment because of federal privacy laws, a spokeswoman said.
It took a week of finagling, but Samuel got his surgeries at Scottish Rite and is recovering in the hospital. Stories like this will continue to flood lawmakers’ email inboxes until the system is fixed, Galinsky said.
“All of us have been so busy taking care of our children and trying to keep them alive that we didn’t have time to get involved in the political process and didn’t notice it until it was thrown in our face, and it was like, ‘Wham,’ ” she said.
“They just decided it was a silent population and they can take away the money and no one will care.”
Published by: The Dallas Morning News
February 13, 2017
J. David McSwane, Data and Enterprise Reporter
Original link: http://www.dallasnews.com/news/texas-legislature/2017/02/13/severely-disabled-kids-risk-texas-enacts-medicaid-cost-savings-plan